Pulmonary care: Expanding the use of Technegas®
Cyclomedica’s commitment to advancing the world of pulmonary diagnostics isn’t limited to our current achievements. Our dedication is mirrored in our relentless pursuit of research, fueling our drive to expand Technegas® indications.
More choices, brighter futures for patients
Technegas® is not just renowned for its role in diagnosing Pulmonary embolism (PE). Our ongoing research and trials delve deeper, exploring its potential in addressing a broader spectrum of respiratory conditions and requirements:
Pulmonary Embolism (PE)
Providing a precise, reliable diagnostic solution for PE, Technegas highlights areas of reduced or blocked blood flow, aiding in the diagnosis of pulmonary embolism.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
Technegas offers a precise, reliable assessment of CTEPH, a rare condition resulting from blood clots in the lungs, by identifying areas of blood flow restriction.
Chronic Obstructive Pulmonary Disease (COPD)
Technegas delivers a precise, reliable evaluation of COPD, enabling clinicians to understand lung function accurately for diagnosis and treatment planning.
Pulmonary Embolism (PE)
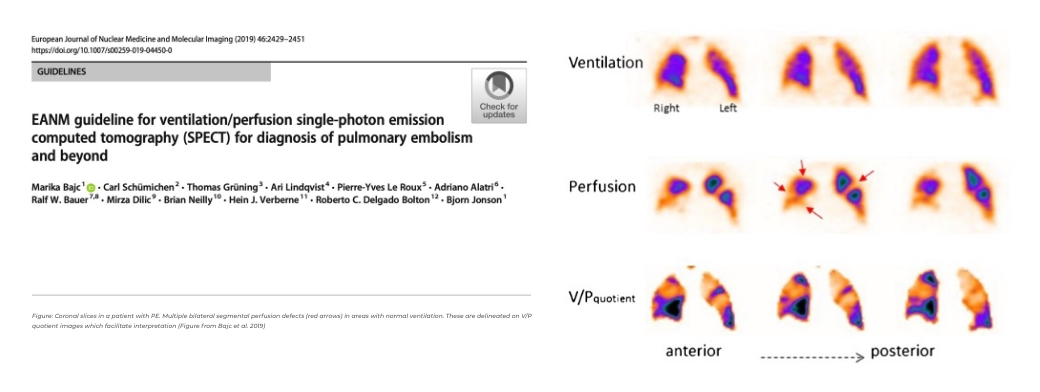
Pulmonary embolism (PE) is a blockage of a pulmonary vessel caused by a blood clot. A mismatch between the ventilation and perfusion scans is an indication of PE.
A lung SPECT scan is a nuclear medicine imaging procedure which uses a radioactive substance and a gamma camera to create 3D pictures showing how lungs work.
- 10 million new cases annually in the world.1
- PE accounts for about one-third of all VTE events.
- 30% of PE are fatal if left untreated2
- Symptoms are varied with diagnosis confirmed either through CTPA or a nuclear medicine ventilation-perfusion study3-4
- V/Q scan should be the initial investigative tool for the diagnosis of PE because it has the highest sensitivity and accuracy and neither contraindications nor complications.5
1. The Global Wolrd Thrombosis Day Movement – Global burden of VTE
2. Bēlohlávek J, et al. Exp Clin Cardiol 2013; 18(2): 129-138
3. Waxman AD, et al. J Nucl Med 2017; 58: 13N-15N
4. Bajc M, et al. Eur J Nucl Med Mol Imaging (2019) 46:2429–2451
5. Hess S, et al. Semin Thromb Hemost 2016; 42(8): 833-845
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
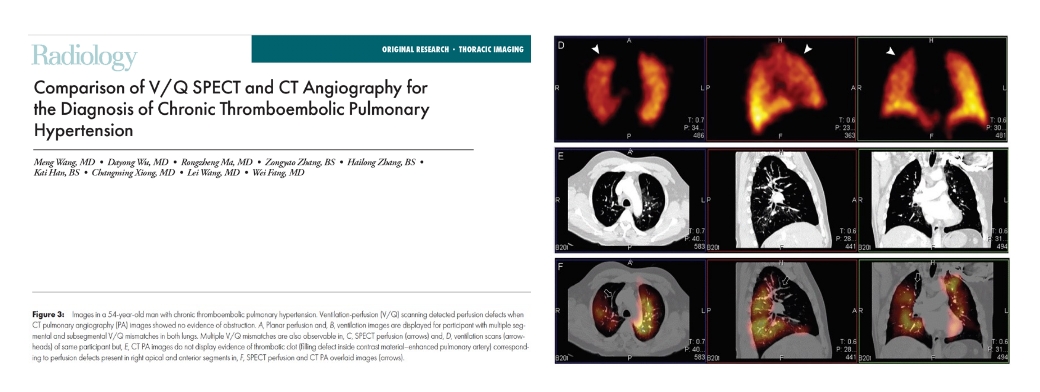
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is a rare and serious medical condition characterized by high blood pressure in the arteries of the lungs (pulmonary hypertension) caused by chronic blood clots or thromboemboli in the pulmonary arteries. Unlike acute pulmonary embolism, where blood clots obstruct the pulmonary arteries suddenly, in CTEPH, these clots fail to dissolve over time, leading to increased pressure in the pulmonary arteries and significant strain on the right side of the heart.
- The current prevalence of CTEPH is between 3000-4000 patients in the USA.1 These figures are rough estimates as only 7-29% of CTEPH cases are diagnosed2.
- If left untreated, CTEPH can lead to heart failure and severe debilitation. The survival rate at 5 years is 30%3.
- V/Q scan is the initial screening test of choice to confirm or rule out CTEPH because if its higher sensitivity compared with CTPA4.
1. Joish V, et al. Chest 2014; 145(3): 523A
2. Gall H, et al. Eur Respir Rev 2017; 26: 160121
3. Tahara N, et al. Diagnosis: Imaging in Fukumoty
4. Konstantinides SV, et al. Eur Heart J 2020; 41(4): 543-603
5. Wang M, et alRadiology 2020; 296(2): 420-429
Chronic Obstructive Pulmonary Disease (COPD)
COPD (Chronic Obstructive Pulmonary Disease) is a progressive and chronic respiratory condition characterized by obstructed airflow in the lungs. This obstruction is typically caused by long-term exposure to irritating gases or particulate matter, such as cigarette smoke. COPD encompasses two main conditions: chronic bronchitis, marked by persistent cough and excess mucus production, and emphysema, involving damage to the lung’s air sacs. COPD leads to symptoms like shortness of breath, coughing, and wheezing, which worsen over time and can significantly impact an individual’s quality of life. Effective management includes smoking cessation, medications, pulmonary rehabilitation, and, in severe cases, oxygen therapy or surgery.
- 18.7 million new cases of COPD per year worldwide 1
- 5% of all deaths
- Each year, 2.9 million people die from COPD 2
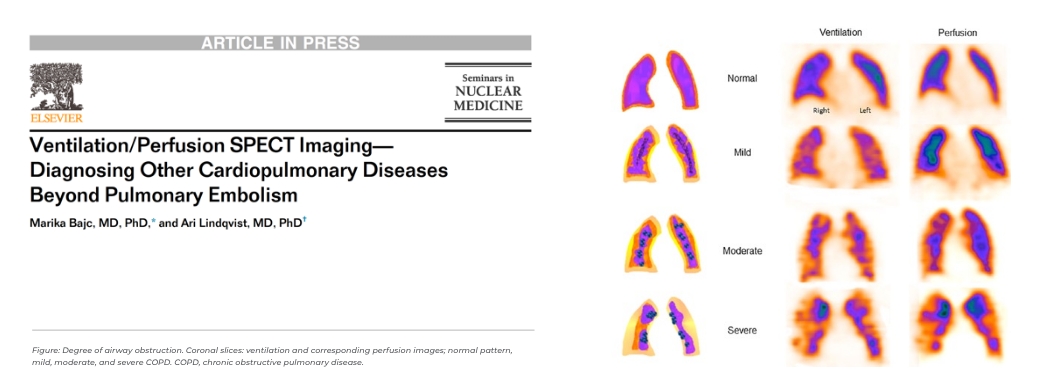
- V/Q can be used as a new tool to clarify the symptoms of patients with COPD, categorize the severity of the disease and monitor treatment efficacy3-4
1.Global Burden of Disease Study 2016
2.Foo J, et al. Plos One 2016; 11(4): e0152618
3.Bajc M, et al. Int J Chron Pulmon Dis 2017; 12: 1579-1587
4.Bajc M, et al. Semin Nucl Med 2019; 49(1): 4-10.